The journey to motherhood is often celebrated for its joy and wonder. However, few conversations touch upon the often-overlooked reality of postpartum pain. From the physical aches of labor and delivery to the emotional turmoil that can accompany a dramatic shift in life, new mothers face a unique set of challenges. Understanding the various types of postpartum pain and developing a comprehensive nursing care plan is crucial for supporting these mothers in their transition to parenthood.

Image: mindbooksdoc.blogspot.com
A postpartum pain care plan aims to not only alleviate discomfort but also to empower mothers with knowledge and tools to manage their pain effectively. This plan is not just about pain relief; it is about fostering a positive postpartum experience, promoting physical recovery, and enabling mothers to bond with their babies without unnecessary physical or emotional distress.
Understanding Postpartum Pain
Types of Postpartum Pain
Postpartum pain manifests in various ways, both physical and emotional. Understanding these different types is the first step in crafting a comprehensive care plan.
- Physical Pain: This can range from mild discomfort to severe pain. Common sources include:
- Episiotomy: A surgical incision made at the opening of the vagina during childbirth.
- Tears: Natural tissue tears that can occur during delivery.
- Hemorrhoids: Swollen veins in the rectum, commonly experienced during pregnancy and postpartum.
- C-Section Incision Pain: Pain associated with the surgical incision made during a C-section.
- Uterine Cramps: Painful contractions of the uterus as it returns to its normal size.
- Breast Engorgement: Painful swelling of the breasts due to milk production.
- Back Pain: Pain in the lower back due to hormonal changes and the strain of labor and delivery.
- Emotional Pain: The emotional transition to motherhood can be overwhelming, leading to:
- Baby Blues: A transient period of mood swings, sadness, and anxiety in the first few days or weeks after delivery.
- Postpartum Depression: A more severe form of depression that can persist for weeks or months after delivery.
- Postpartum Anxiety: Excessive worry and fear related to the baby’s health, parenting abilities, or other concerns.
Factors Influencing Postpartum Pain
A number of factors can influence the severity and duration of postpartum pain. Recognizing these factors allows nurses to tailor their pain management strategies:
- Type of Delivery: Vaginal deliveries often lead to pain in the perineal area, while C-sections result in pain at the incision site.
- Pain Threshold: Individual pain tolerance levels vary significantly.
- Previous Experiences: Past experiences with pain can affect how a woman perceives and manages postpartum pain.
- Emotional State: Stress, anxiety, and fatigue can intensify pain perception.
- Cultural Factors: Cultural beliefs and practices can influence how women express and manage their pain.
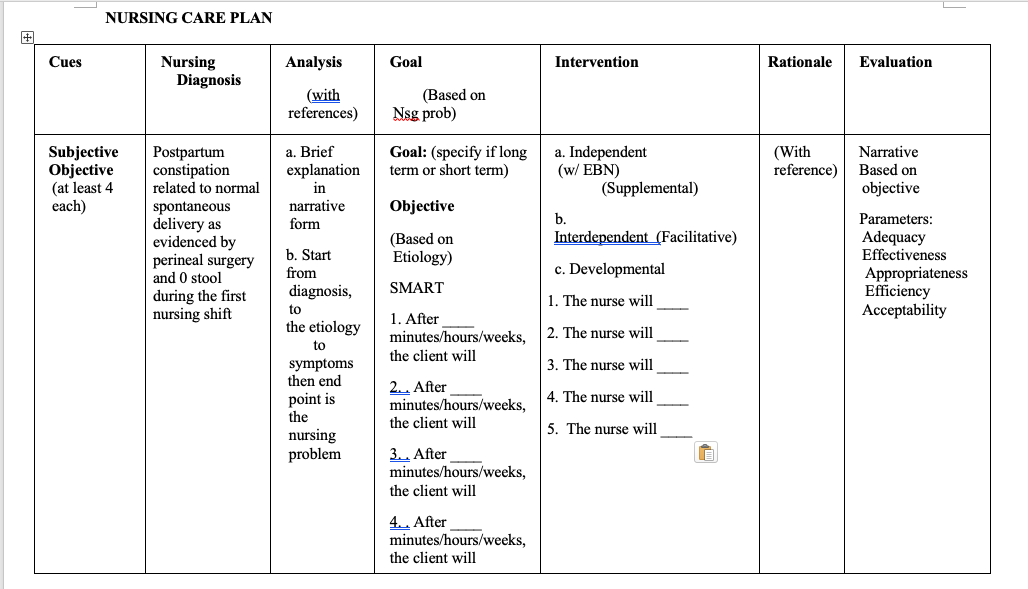
Image: www.hotzxgirl.com
The Nursing Care Plan: A Multi-faceted Approach
A well-structured nursing care plan addresses postpartum pain holistically, encompassing both physical and emotional needs. It involves assessment, interventions, evaluation, and ongoing communication.
Assessment: Recognizing the Individual Experience
The first step is a thorough pain assessment, conducted upon admission and regularly throughout the postpartum period:
- Location and Intensity of Pain: Using tools like the numeric pain scale or visual analog scale can be helpful.
- Quality of Pain: Is it sharp, throbbing, aching, or burning?
- Duration of Pain: Is it constant or intermittent? How long does it last?
- Factors that Aggravate or Relieve Pain: Understanding these factors can help tailor the care plan.
- Impact of Pain on Daily Activities: How is the pain affecting the mother’s ability to care for herself and her baby?
- Emotional Response to Pain: Is the mother frustrated, anxious, or depressed about the pain?
Interventions: Tools for Pain Management
The nursing care plan will then outline interventions to address the specific pain experienced by each mother. These may include:
- Pharmacological Interventions:
- Analgesics: Over-the-counter or prescription pain relievers, such as ibuprofen or acetaminophen, can be used safely during breastfeeding.
- Opioids: If pain is severe, opioids may be prescribed, but their use is typically short-term due to the potential for dependence.
- Epidural Analgesia: This method can provide pain relief for several days after delivery, particularly after a C-section.
- Non-Pharmacological Interventions:
- Heat or Cold Therapy: Applying heat or cold packs to the affected area can help reduce pain and swelling.
- Massage: Gentle massage can ease muscle tension and improve blood circulation.
- Positioning: Finding comfortable positions for sitting, lying down, and breastfeeding can minimize pain.
- Rest and Relaxation: Getting enough rest and practicing relaxation techniques like deep breathing or meditation can promote healing and reduce pain perception.
- TENS Unit: Transcutaneous electrical nerve stimulation (TENS) units use low-voltage electrical currents to block pain signals.
- Perineal Care: Proper hygiene and wound care are essential for promoting healing and preventing infection after vaginal delivery or episiotomy:
- Sitz Baths: Sitz baths can help soothe and clean the perineal area.
- Ice Packs: Applying ice packs to the area can reduce swelling and bruising.
- Warm Compresses: Warm compresses can help relax muscles and relieve pain.
- Perineal Spray: Specialized sprays can help keep the area clean and prevent infection.
- Witch Hazel: This natural astringent can help reduce swelling and discomfort.
- Emotional Support: Nurses play a vital role in providing emotional support and coping strategies:
- Active Listening: Nurses should actively listen to the mother’s concerns, fears, and anxieties.
- Empathy: Empathy is key. Nurses should show genuine care and understanding for the mother’s unique experience.
- Education: Providing accurate and helpful information about postpartum pain can empower mothers to manage their own care.
- Referral: If a mother exhibits signs of postpartum depression or anxiety, a referral to a mental health professional is crucial.
Evaluation: Monitoring and Adjusting the Plan
The nursing care plan is not static. Nurses need to regularly evaluate its effectiveness and make adjustments as needed based on the mother’s progress.
- Pain Assessment: Regular pain assessments allow nurses to track the effectiveness of interventions.
- Observations: Nurses should carefully observe the mother’s behavior, verbal cues, and nonverbal signals to gauge her pain level.
- Communication: Open communication is vital. Nurses should encourage the mother to express her experience and any concerns she may have.
- Documentation: Thorough documentation of pain assessments, interventions, and responses is essential for continuity of care.
The Importance of Patient Education and Empowerment
Nurses play a critical role in empowering mothers to manage their pain effectively. This involves providing education and resources to help them understand and cope with their postpartum experience.
- Pain Management Techniques: Nurses should teach mothers about various pain management techniques, including relaxation techniques, breathing exercises, and positioning strategies.
- Medication Instruction: Nurses should provide clear instructions on how to take prescribed medications, including dosages, timing, and side effects.
- Self-Care Practices: Nurses should encourage mothers to prioritize self-care practices such as getting enough rest, eating nutritious food, and staying hydrated.
- Community Resources: Nurses should make mothers aware of available community resources, such as support groups, lactation consultants, and mental health professionals.
Nursing Care Plan For Postpartum Pain
https://youtube.com/watch?v=nOgPCEHIw18
Conclusion: A Collaborative Approach to Promoting Well-being
A comprehensive nursing care plan for postpartum pain is essential for ensuring the well-being of new mothers. By understanding the various types of pain, assessing individual experiences, and implementing effective interventions, nurses can provide personalized care that addresses both physical and emotional needs. The ultimate goal is to empower mothers with knowledge, support, and resources to navigate this transformative period with confidence and comfort. Remember that every woman’s postpartum experience is unique and requires a sensitive, collaborative approach that prioritizes individual needs and promotes a smooth transition to motherhood.






