Have you ever noticed a tinge of yellow in a newborn’s skin? This is a common phenomenon known as neonatal jaundice, and while it can be a cause for concern, most cases are harmless and resolve on their own. However, understanding the causes, symptoms, and effective nursing care for this condition is essential for ensuring the well-being of your little one. Join us as we delve into the world of neonatal jaundice, its nursing care plan, and the crucial role nurses play in managing this condition.
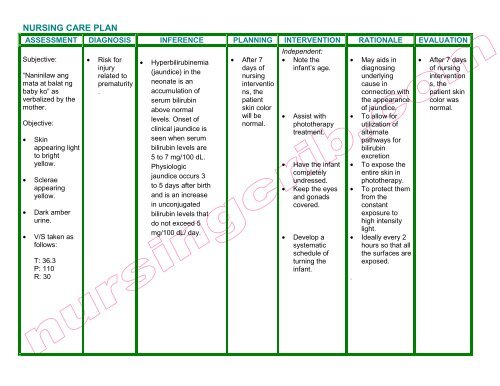
Image: mungfali.com
Neonatal jaundice is a condition that occurs when there is an excessive amount of bilirubin, a yellow pigment, in a newborn’s blood. Bilirubin is a natural byproduct of the breakdown of red blood cells. Normally, it’s processed by the liver and excreted in the stool. However, in newborns, the liver may not be fully developed, leading to a build-up of bilirubin, which causes the skin and whites of the eyes to appear yellow.
Understanding the Causes of Neonatal Jaundice
Physiological Jaundice:
This is the most common type of jaundice, affecting about 60% of full-term newborns and almost all preterm infants. This type is usually caused by the baby’s immature liver not being able to process bilirubin efficiently. It typically appears on the second or third day of life and gradually fades within a week or two.
Breastfeeding Jaundice:
This type of jaundice occurs in breastfed babies, particularly those who are feeding poorly or not getting enough breast milk. This can lead to a decrease in stool frequency, which can cause bilirubin levels to rise. It usually begins around the third or fourth day of life and can last for several weeks.

Image: www.youtube.com
Breast Milk Jaundice:
While similar to breastfeeding jaundice, this type is caused by a specific substance in breast milk that can interfere with bilirubin breakdown. It typically appears after the first week of life and can last for several weeks or even months. While these babies may require extra monitoring, it does not affect the baby’s health or the mother’s ability to breastfeed.
Pathological Jaundice:
This less common type of jaundice is caused by an underlying medical condition, such as blood incompatibility, infection, or liver disease. It usually appears within the first 24 hours of life and may require immediate medical attention. These conditions may require medical intervention and may not resolve on their own.
The Nursing Care Plan for Neonatal Jaundice
Assessing for Jaundice:
Nurses play a critical role in assessing newborns for jaundice. Regular skin and sclera (whites of the eyes) examinations are paramount. Since bilirubin levels are highest in the morning, these assessments are often done first thing in the day.
Monitoring Bilirubin Levels:
The nurses will monitor bilirubin levels using a transcutaneous bilirubinometer (TCB) or blood tests. This helps them determine the severity of the jaundice and inform the appropriate treatment plan.
Encouraging Feeding:
Frequent feedings are crucial to help the baby pass meconium, the first stool, which aids in bilirubin elimination. Nurses provide guidance and support to mothers on breastfeeding techniques and ensuring the baby receives adequate nutrition.
Phototherapy:
For babies with moderate to severe jaundice, phototherapy is often recommended. This non-invasive treatment involves exposing the baby to blue light, which helps break down bilirubin in the blood. Nurses will closely monitor the baby’s temperature and hydration during phototherapy sessions. It’s important to note that the baby is naked while receiving this therapy and must be monitored closely and kept warm.
Exchange Transfusion:
In rare cases, if jaundice is severe and phototherapy is ineffective, an exchange transfusion may be necessary. This procedure involves replacing the baby’s blood with fresh donor blood, which reduces the bilirubin levels.
Educating Parents:
Nurses play a crucial role in educating parents about neonatal jaundice. By explaining the cause, symptoms, treatment options, and potential complications, they empower parents to be active participants in their baby’s care.
Importance of Early Intervention
Early intervention is essential in managing neonatal jaundice. When diagnosed and treated promptly, most cases can be resolved without complications. The severity of jaundice varies depending on the bilirubin level and the baby’s age. Without treatment, high bilirubin levels can lead to kernicterus, a serious condition that can damage the brain.
Nursing Considerations
Monitoring Vital Signs:
Nurses continuously monitor the baby’s vital signs, including temperature, heart rate, respiratory rate, and blood pressure, during treatment, particularly those receiving phototherapy.
Hydration Management:
Adequate hydration is essential for babies, especially those receiving phototherapy, as it promotes bilirubin excretion through urine. Nurses monitor fluid intake and output, ensuring the baby receives enough fluids.
Skin Assessment:
Regular skin assessment is critical to identify any signs of complications, such as skin breakdown or rashes, which can occur with phototherapy or due to frequent diaper changes.
Nursing Care Plan For Neonatal Jaundice
Conclusion
Neonatal jaundice is a common condition that can be effectively managed with prompt and appropriate nursing care. Understanding the causes, symptoms, and treatment options is essential for nurses to provide optimal care for the baby and support the parents. By diligently monitoring bilirubin levels, encouraging frequent feedings, providing phototherapy, and ensuring adequate hydration, nurses play a vital role in ensuring a positive outcome for babies with jaundice. Remember that open communication with parents and a comprehensive care plan can help alleviate anxieties and encourage a peaceful transition into parenthood.






