Imagine waking up one morning, unable to move your legs or even get out of bed. This is the reality for many individuals facing impaired physical mobility, a condition that affects their ability to move about freely and independently. It’s a common challenge encountered in healthcare settings, impacting a significant portion of the population. Navigating this challenge requires a tailored approach, often involving a nursing care plan that focuses on maximizing the individual’s functional abilities and promoting their overall well-being.

Image: rosepdfs.blogspot.com
This article will delve into the intricacies of a nursing care plan for impaired physical mobility, providing a comprehensive guide to understanding and implementing effective interventions. We will explore the principles guiding such plans, delve into specific care strategies, and highlight the importance of collaborative teamwork in achieving optimal patient outcomes. By understanding the complexities of this topic, you can gain valuable insights into how healthcare professionals support individuals facing impaired mobility challenges.
Understanding Impaired Physical Mobility
Impaired physical mobility encompasses a range of limitations in movement, including decreased range of motion, weakness, pain, and difficulty with balance and coordination. This can arise from various underlying conditions such as stroke, spinal cord injury, musculoskeletal disorders, and even prolonged bed rest. The impact of impaired mobility extends beyond the physical realm, affecting an individual’s daily activities, independence, and overall quality of life.
Assessing the Individual’s Needs
The foundation of any effective nursing care plan lies in a thorough assessment. Nurses must gather comprehensive information about the individual’s mobility limitations, including their current functional status, pain levels, cognitive abilities, and any existing medical conditions. This assessment forms the basis for developing personalized goals and interventions.
Key Assessment Areas:
- Musculoskeletal System: Examining joint range of motion, muscle strength, and any signs of pain or inflammation.
- Neurological Functioning: Evaluating balance, coordination, reflexes, and sensory perception.
- Cardiovascular Status: Assessing heart rate, blood pressure, and any respiratory difficulties that might arise during movement.
- Cognitive Abilities: Understanding the individual’s ability to follow instructions, make decisions, and participate in their care planning.
- Social and Environmental Factors: Considering the individual’s living situation, support network, and any potential barriers to mobility.
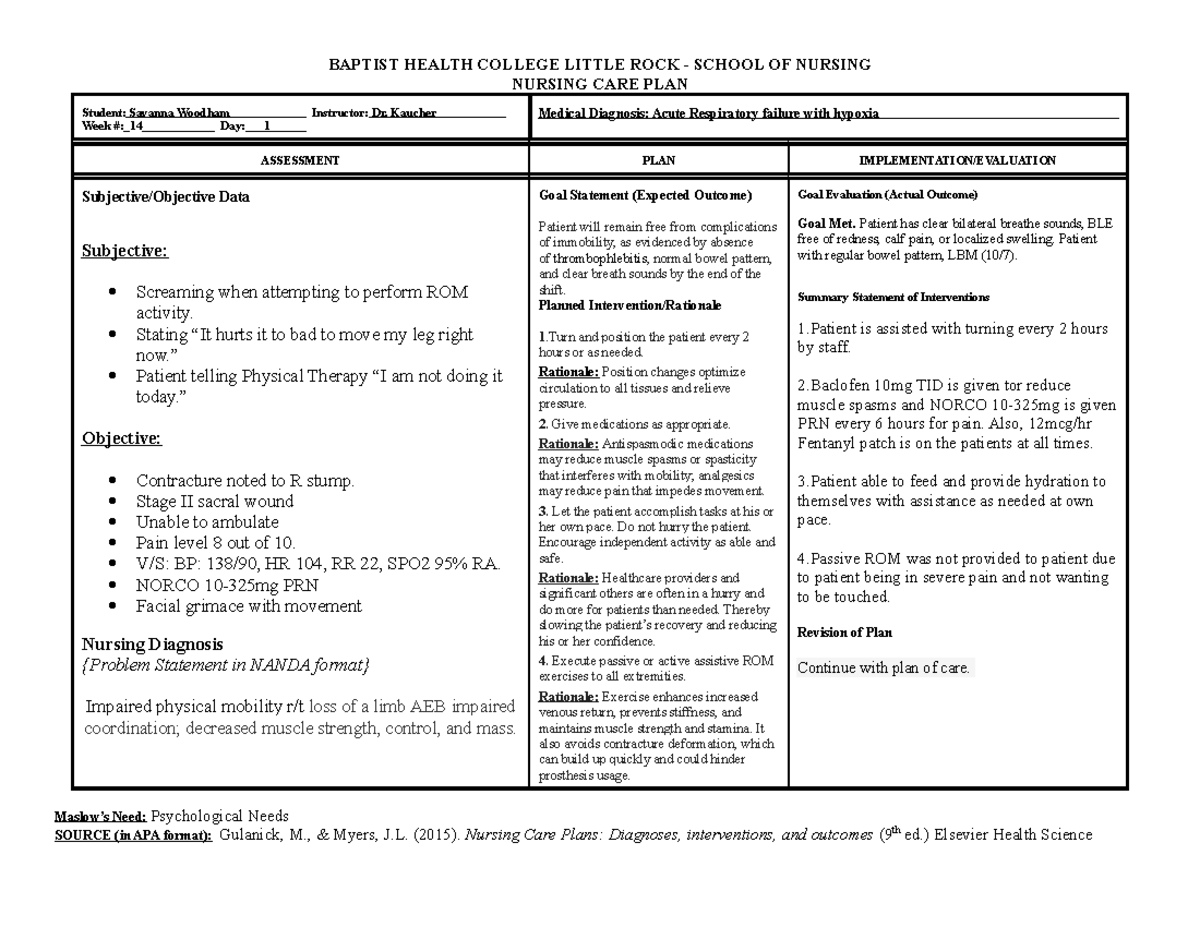
Image: www.studocu.com
Developing a Nursing Care Plan
Once the assessment is complete, nurses collaborate with the individual, their family, and other healthcare professionals to develop a comprehensive care plan that addresses their specific needs. This plan outlines the goals, interventions, and strategies for promoting optimal mobility and independence.
Setting Realistic Goals
The goals set within the care plan should be realistic, measurable, attainable, relevant, and time-bound (SMART). They should focus on improving the individual’s functional abilities, reducing pain, enhancing safety, and promoting overall well-being. For example, a goal might be to increase the individual’s walking distance by 50 feet within two weeks.
Implementing Interventions
A variety of interventions can be utilized to enhance mobility and address specific challenges. These may include:
Physical Therapy and Exercise:
Physical therapists play a crucial role in designing individualized exercise programs that target muscle strengthening, range of motion improvement, and balance training. Regular exercise is essential to maintain and improve functional abilities. These exercises can vary from simple stretches to more complex resistance training depending on the individual’s capabilities.
Assistive Devices:
Assistive devices such as canes, walkers, crutches, wheelchairs, and specialized footwear can provide support and stability, enabling individuals to move more safely and independently. The appropriate assistive device is determined based on the individual’s needs and the specific challenges they face.
Environmental Modifications:
Modifications to the individual’s home environment, such as removing tripping hazards, installing grab bars, and elevating toilet seats, can significantly enhance safety and improve accessibility. Addressing environmental obstacles can help create a more supportive and conducive setting for mobility.
Pain Management:
Pain can severely hinder mobility and limit an individual’s participation in activities. Pain management strategies may include medications, heat or cold therapy, and relaxation techniques. Effective pain relief enables individuals to engage more actively in physical therapy and other rehabilitation activities.
Positioning and Skin Care:
Proper positioning is critical to prevent pressure ulcers and promote circulation. Regular turning, pressure relief measures, and meticulous skin care are essential for individuals with limited mobility. This includes ensuring appropriate bedding and using specialized mattresses or cushions to distribute pressure evenly.
Education and Support:
Nurses play a vital role in educating individuals and their families about mobility strategies, assistive devices, and home safety measures. Providing clear instructions and demonstrating proper techniques empowers individuals to actively participate in their care and maintain their independence. The role of support from family and friends cannot be underestimated. Encouraging a network of support is key to promoting a positive mindset and fostering a sense of independence.
Fall Prevention:
Falls are a significant risk for individuals with impaired mobility, leading to injuries and further limitations. Nurses implement strategies to minimize the risk of falls, such as ensuring adequate lighting, removing tripping hazards, using assistive devices, and providing close supervision when necessary.
Collaboration with Other Healthcare Professionals:
Nurses collaborate closely with physical therapists, occupational therapists, physicians, and other team members to ensure a coordinated approach to care. Sharing information about the individual’s progress and challenges helps ensure effective and seamless treatment. This collaborative approach is vital to optimize patient outcomes and promote holistic care.
Ongoing Monitoring and Evaluation
The nursing care plan is not a static document; it needs to be continuously evaluated and adjusted as the individual’s condition and capabilities change. Regularly monitoring the individual’s progress, assessing their response to interventions, and making adjustments as needed is essential to ensure ongoing effectiveness.
Key Evaluation Measures:
- Functional Independence: Assessing the individual’s ability to perform daily activities such as dressing, bathing, and transferring.
- Pain Levels: Monitoring changes in pain intensity and frequency.
- Range of Motion: Quantifying improvements in joint movement.
- Fall Risk: Evaluating the individual’s risk factors for falls and implementing appropriate precautions.
Adapting the Nursing Care Plan
As individuals with impaired physical mobility progress, their needs may change. The care plan must be flexible and adaptable to accommodate these changes. For example, as an individual gains strength and coordination, the intensity of their exercise program might be increased. Similarly, if their mobility improves, the type or level of assistance required may be reduced.
Importance of Patient Centered Care
A critical aspect of any effective nursing care plan is that it is patient-centered. This means that the individual’s needs, preferences, and goals are at the forefront of the care planning process. Providing individuals with choices and involving them in decision-making regarding their care promotes their sense of autonomy and enhances their overall well-being.
Example of a Nursing Care Plan
Let’s consider a hypothetical example of a nursing care plan for an individual who has recently experienced a stroke and has impaired mobility on the left side of their body.
Patient: John Smith, 65-year-old male
Diagnosis: Stroke, left hemiparesis
Goals:
- Improve left-sided strength and mobility within 4 weeks.
- Increase walking distance to 100 feet without assistance within 6 weeks.
- Maintain skin integrity, free from pressure ulcers, throughout hospitalization.
Interventions:
- Collaborate with physical therapist for individualized exercise plan, focusing on left-sided strengthening and range of motion exercises.
- Provide assistive devices such as a cane or walker to improve stability and support during walking.
- Educate John and family on safe transfer techniques using a gait belt.
- Implement fall prevention measures, including clear walkways, adequate lighting, and close supervision when necessary.
- Perform regular skin assessments and Implement pressure relief measures, including turning schedule and use of a pressure-reducing mattress.
Evaluation:
- Monitor John’s progress with exercises and walking distance.
- Assess pain levels and effectiveness of any pain management interventions.
- Evaluate skin condition for any signs of breakdown or pressure ulcers.
- Adjust care plan as needed based on John’s progress and individual needs.
Example Of Nursing Care Plan For Impaired Physical Mobility
Conclusion
A nursing care plan for impaired physical mobility plays a vital role in supporting individuals facing these challenges. The plan should be tailored to their specific needs, goals, and preferences. It involves a comprehensive assessment, collaborative goal setting, implementation of targeted interventions, ongoing monitoring, and adaptation based on the individual’s progress. Providing patients with education, support, and a sense of autonomy enhances their overall well-being and empowers them to regain function and live fulfilling lives.






